Teams spend 60% of audit prep manually gathering compliance evidence, increasing errors and costs.
SaaS solutions expose patient data to third-party vendors and compliance violations, requiring complex BAAs.
CMS RADV audits expanded from 60 to 550+ plans with $400M+ recovery exposure for Payors.
AI pilots fail due to missing governance and explainability frameworks for auditors.
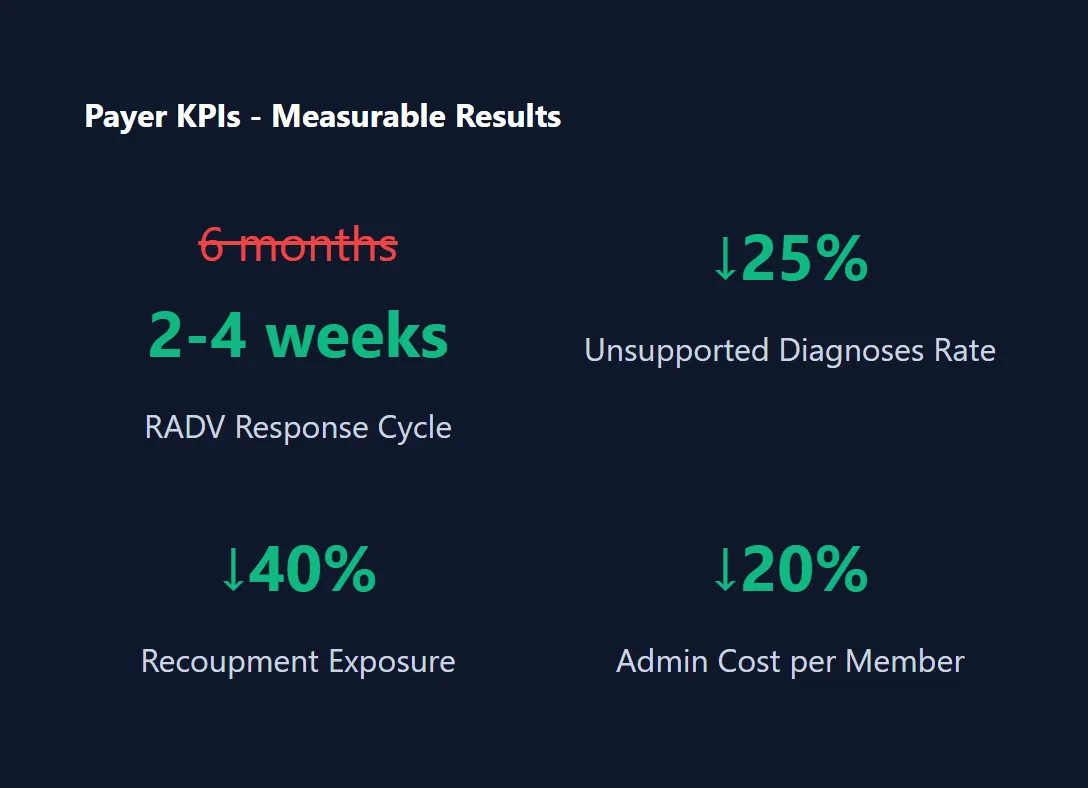

Orchestrates record requests, ingests documents, links diagnoses to documentation, and exports CMS-ready packets with citations and acceptance logs. Automated workflow manages the entire RADV audit response process.

Continuous agent scans for unsupported coding with provider feedback loops. Real-time validation of hierarchical condition categories against medical documentation ensures coding accuracy.

BAAs/DUAs normalization and PHI-sharing controls across delegated entities with continuous monitoring tie-ins. Automated vendor risk assessment and compliance tracking.

AI-driven validation improving first-pass accuracy and reducing denials. Predictive analytics identify potential issues before claims submission.


On-demand evidence collection with policies, access logs, training records, and risk assessments. Automated assembly of comprehensive HIPAA audit response packages.

Watch physician-entity relationships, flag violations, enforce HITL approvals. Continuous monitoring of financial arrangements and referral patterns.

Detect shadow suppliers, align data use agreements, track remediation SLAs. Automated vendor risk assessment and compliance monitoring.

All processing in your network with model-agnostic flexibility. Complete control over patient data with zero third-party exposure.
| Solution Category | Traditional Approach | InteliGems Advantage |
|---|---|---|
| Big 4 Consulting | $500K-$2M annually, 6-12 month timelines, manual processes | 70% lower TCO, 1-4 week deployment, continuous automation |
| SaaS GRC Platforms | PHI in vendor clouds, ongoing licensing, limited customization | Complete PHI sovereignty, zero licensing fees, unlimited customization |
| Healthcare AI Vendors | Clinical focus only, complex integrations, vendor lock-in | Compliance-specific architecture, proven regulatory frameworks, platform ownership |
| Internal Development | 80-95% failure rate, $1M-$5M investment, 12-36 month timelines | 70% lower cost, 1-4 week deployment, 97% accuracy guarantee |
From Strategy to Audit-Ready Operations in 4 Weeks

Get started today
Partner with experts who understand your compliance goals and help you achieve lasting success with AI-powered solutions. Let's build a strategy tailored to your needs.